The Facts About How Much Would Universal Health Care Cost Uncovered
The 2010 Affordable Care Act included more agencies to this list, including state Alcohol Abuse Treatment insurance exchanges and the Center for Medicare and Medicaid Innovation. Each location of healthcare has its own intricacies. As elements of the bigger healthcare system interact, the complex layers unfold. While change is anticipated in the coming years, it is likely to happen gradually.
For example, the methods clients and administrators use resources such as Medicare and Medicaid have actually changed due to legislation. Technology has had a further effect on how healthcare administrators handle resources and manage medical centers. Cultural shifts, expense of care, and policy adjustments have contributed to a more patient-empowered shift in care over the last century.

This trend is anticipated to continue as brand-new health care electronic technologies, such as 3D printing, wearable biometric devices, and GPS tracking, are tested and introduced for scientific use. Policies and treatments in specific facilities might limit how and when new innovations are introduced, however cutting-edge technology is expected to play an increasingly larger role in our healthcare system within the coming years.
This development is due to an anticipated boost in Medicare beneficiaries in the coming years. The expense of medical facility care is expected to increase from 0. 9 percent to 2. 4 percent of the budget by 2025, increasing the importance of good company practices and educated specialists in the healthcare industry.
Because then, Addiction Treatment Center Congress has actually made Medicare and Medicaid modifications to open eligibility to more individuals. For instance, Medicare was expanded in 1972 to cover the handicapped, individuals over 65, and others. Medicare includes more benefits today, consisting of unlimited house health check outs and quality standards for Medicare-approved retirement home. Medicaid has actually also been broadened to cover a larger group than initially meant.
Wide variations in Medicaid programs across the country occur because specific states have the ability to customize Medicaid programs to serve the needs of their homeowners. In 2010, the Affordable Care Act presented the Health Insurance coverage Market, which has had a direct effect on Medicaid service. Potential customers can now utilize the Marketplace website to determine their Medicaid eligibility.
Assuming the federal government continues to support Marketplace premiums for lower-income populations, this increased government healthcare spending will greatly affect the entire health care system in the U.S. Although Medicaid spending growth decreased in 2016 due to lowered enrollment, costs is anticipated to speed up at an average rate of 7. 1 percent per year in 2018 and 2019 due to the aging infant boomer generation.
What Is A Health Care Premium Can Be Fun For Anyone
Providers are a vital part of the health care system and any changes to their education, satisfaction or demographics are https://penzu.com/p/6f3a01b2 likely to affect how patients receive care. Future doctor are likewise most likely to focus their education on service than ever in the past. A massive analysis of Harvard Service School's doctor graduates suggests substantial development in the number of doctors pursuing M.B.A.
This development might result in more private practices and healthcare administrators. Over the last few years, the demographics of the medical occupation have actually shifted. Ladies currently make up most of health care suppliers in specific specialties, consisting of pediatrics and obstetrics and gynecology. Nearly one-third of all practicing doctors are women. According to an Association of American Medical Colleges (AAMC) analysis, females make up 46 percent of all doctors in training and almost half of all medical trainees.
African-American females are most likely to end up being doctors than their male equivalents, according to AAMC data. While African-Americans make up just four percent of the physician workforce, 55 percent of the African American doctor workforce is female. This shift in demographics to consist of more women in healthcare supports variety in the market and represents general population variety.
The quantity of malpractice claims in the U.S. has actually progressively decreased given that 2004. As the pattern of declining malpractice claims continues, it may show that company competence and patient care will continue to improve. Job complete satisfaction is one location that must improve. According to Medscape's 2015 Doctor Payment Report, 64 percent of doctors would choose medicine as a profession if they could do it once again, however just 45 percent would select the very same area of specialty.
9 out of 10 nurses who participated in the survey stated they were satisfied with their career choice. However, one out of every 3 nurses is unhappy with their present job. It is tough to state whether job complete satisfaction will increase in the coming years, however continued technological developments developed to streamline the healthcare process deal hope to those who may be annoyed with the intricacy of their jobs.
Every year, new treatments and treatments assist handle common diseases. Each such development affects the entire healthcare system as much as it has a favorable effect on patients. As diseases end up being more typical, our health care system need to adjust to treat them. Patient care needs will also develop as the population ages and relies more heavily on resources such as Medicare and Medicaid.
The bubonic pester is a great example of a disease that can considerably alter the healthcare system by rapidly shifting all resources to manage an epidemic. In the Middle Ages, the Black Death spread out so quickly across Europe that it is accountable for an approximated 75 million deaths. It may be unexpected that the bubonic afflict still circulates today.
The Only Guide to Why Single Payer Health Care Is Bad
within 5 months in 2015. what is a health care delivery system. Although the bubonic afflict is not near the threat it once was, other diseases and conditions of concern are on the increase. The following seven conditions are on the rise and can be anticipated to have an effect on healthcare in the near future: Chlamydia and gonorrhea rates have actually increased, and syphilis rates rose by 15.
Obesity continues to be a concern in the U.S. with 78. 6 million adults and 12. 7 million children affected. Weight problems rates have actually increased by 17 percent in the previous five years. For every single 100,000 people, 1,470 are diagnosed with autism. This number continues to rise every year. Recent boosts may be because of awareness as medical professionals end up being more familiar with the symptoms of autism.
coli have increased by 472 percent. Lots of E. coli cases are the outcome of food contamination. Incidences of liver cancer have actually increased by 47 percent in a recent 10-year timeframe. Healthcare practitioners have treated 18. 6 percent more cases of kidney cancer in the past ten years than in previous years.
This may be due in part to moms and dads pulling out of whooping cough vaccinations. The healthcare industry has actually determined these previous conditions, preparing to handle further increases with supplies and resources. However, a new risk is constantly possible. If something similar to the Ebola virus spread across the country, this would have a drastic effect on client care and healthcare facilities.
9 percent in 2018 and 2019. Healthcare innovation trends focus heavily on patient empowerment. The introduction of wearable biometric gadgets that provide patients with information about their own health and telemedicine apps permit patients to easily access care no matter where they live. With new technologies concentrated on monitoring, research, and health care accessibility, clients will be able to take a more active function in their care.
7 Easy Facts About How Did The Patient Protection And Affordable Care Act Increase Access To Health Insurance? Explained
Individuals who are covered under employer-sponsored health strategies or private market health insurance in the U.S. (including ACA-compliant plans) are not part of a single-payer system, and their health insurance is not government-run. In these markets, hundreds of separate, personal insurance companies are accountable for paying members' claims. In many cases, universal protection and a single-payer system go hand-in-hand, because a nation's federal government is the most likely prospect to administer and spend for a healthcare system covering millions of people.
Nevertheless, it is very possible to have universal coverage without having a complete single-payer system, and various nations around the globe have actually done so. Some nations run a in which the government supplies standard health care with secondary protection readily available for those can manage a higher requirement of care. Two-thirds of Canadians, for example, purchase extra personal protection for dental, vision, and prescription drugs, due to the fact that the government-run plan does not offer those advantages.
This resembles Medigap coverage in America, for people covered under Original Medicare. The federal government offers Original Medicare protection, however it does not have a cap on how high out-of-pocket expenses can be. So most Original Medicare recipients count on some form of extra coveragefrom an employer or former employer, Medicaid, or privately-purchased Medigap policies.
In a socialized medicine system, the government not only spends for healthcare however runs the medical facilities and employs the medical personnel. A country can adopt a single-payer technique (ie, the government pays for treatment) without a socialized medicine approach. The National Health Service (NHS) in the UK is an example of a system in which the government spends for services and likewise owns the medical facilities and utilizes the doctors.
They simply bill the federal government for the services they provide, much like the American Medicare program. The primary barrier to any socialized medication system is the federal government's ability to efficiently fund, manage, and update its requirements, devices, and practices to offer optimal healthcare. Some specialists have actually recommended that the United States ought to incrementally reform its existing health care system to provide a government-funded safeguard for the ill and the bad (sort of an expanded version of the ACA's Medicaid growth) while needing those who are more lucky health-wise and economically to buy their own policies.
But it is technically possible to construct such a system, which would provide universal coverage while also having several payers. While it is theoretically possible to have a national single-payer system without likewise having universal health coverage, it is very unlikely to ever occur because the single-payer in such a system would undoubtedly be the federal government.

federal government were to embrace such a system, it would not be politically feasible for them to leave out any private resident from health coverage. Despite this, a growing variety of congressional representatives have called for the establishment of "Medicare for All," a proposal popularly endorsed by the advocates of Vermont Senator Bernie Sander in his governmental projects.
About How To Take Care Of Mental Health
government would supply protection to all American citizens, there are various approaches that have been proposed and they would all consist of more robust protection than the current Medicare program supplies. These methods have actually been improperly labeled "socialist" by most in the Republican Party, however none of the present Medicare for All proposals would integrate socialized medicine.
The majority of them have achieved universal protection with one hundred percent of their population covered by core health advantages. However in 7 of the nations (Chile, Estonia, Hungary, Mexico, Poland, the Slovak Republic, and the United States), less than 95% of the population has thorough health coverage. According to current U.S.
population was insured in 2019. The U.S. is near the bottom of the OECD countries in regards to the percentage of its citizens with health protection, however it likewise invests even more of its GDP on health care than any of the other member countries. Let's have a look at the numerous methods that some countries have achieved universal or near-universal coverage: Germany has universal protection however does not operate a single-payer system.
Most workers in Germany are instantly registered in one of more than 100 non-profit "sickness funds," paid for by a combination of worker and company contributions. Additionally, there are private medical insurance prepares available, however only about 10% of German homeowners pick private medical insurance. Singapore has universal coverage, and big health care expenses are covered (after a deductible) by a government-run insurance system called MediShield.

5% of their earnings to a MediSave account. When patients need regular healthcare, they can take money out of their MediSave accounts to pay for it, but the cash can only be utilized for specific expenses, such as medications on a government-approved list. In Singapore, the government straight subsidizes the expense of health care instead of the expense of insurance coverage (on the other hand with the technique that the United States takes with protection acquired through the ACA health exchanges, in which the cost of the medical insurance is subsidized).
design. Japan has universal coverage but does not utilize a single-payer system. Protection is primarily offered via countless completing health insurance strategies in the Statutory Medical Insurance System (SHIS). Residents are needed to register in coverage and pay continuous premiums for SHIS coverage, however there is also an alternative to purchase personal, extra health insurance coverage.
The United Kingdom is an example of a nation with universal coverage and a single-payer system. Technically speaking, the U.K. model can also be classified as socialized medication given that the government owns the majority of the health centers and employs the medical providers. Funding for the U.K. National Health Service (NHS) originates from tax income.
The 30-Second Trick For Who Is Eligible For Care Within The Veterans Health Administration?
It can be used for elective treatments in personal hospitals or to get faster access to care without the waiting duration that might otherwise be imposed for non-emergency scenarios.
In a single-payer system, one entity would act as an administrator or payer. This entity would collect all health care fees and pay all health expenses, and all providers (e. g., medical facilities, doctors and other professionals) would bill one entity for their services. Patients would have an option over their suppliers, who would remain as independent as they are today.
A single-payer system would significantly simplify administration, therefore cutting down on documentation and permitting more cash to go towards real medical services. In addition, enhanced databases would allow better monitoring of usage patterns, allowing the recognition of geographical areas in which services are over- or under-utilized. This system has been approximated to lower administrative services from the existing 25-30 percent of the superior dollar under personal insurance coverage to around 5 percent - who is eligible for care within the veterans health administration?.
( Source: and National Nurses Organizing Committee.) Universal means access to healthcare for everyone, period. Even if you are jobless, or lose or alter your task, your health https://www.google.com/maps/d/edit?mid=1w5nqIF84BryTAbjUdxqs4Z7tr2GiUY_I&usp=sharing coverage goes with you. No Cadillac plans for the rich and Moped strategies for everyone else, with high deductibles, minimal services, caps on payments for care, and no security in the occasion of a catastrophe.
The 15-Second Trick For Which Statement About Gender Inequality In Health Care Is True?
This is based upon risk pooling. The social health insurance model is also described as the Bismarck Design, after Chancellor Otto von Bismarck, who presented the first universal health care system in Germany in the 19th century. The funds normally contract with a mix of public and personal providers for the arrangement of a defined benefit package.
Within social medical insurance, a number of functions may be executed by parastatal or non-governmental sickness funds, or in a couple of cases, by personal medical insurance business. Social medical insurance is utilized in a variety of Western European countries and increasingly in Eastern Europe in addition to in Israel and Japan.
Private insurance coverage includes policies sold by commercial for-profit firms, non-profit companies and community health insurers. Normally, private insurance is voluntary in contrast to social insurance programs, which tend to be obligatory. In some nations with universal protection, personal insurance frequently leaves out certain health conditions that are expensive and the state health care system can supply protection.
In the United States, dialysis treatment for end stage renal failure is normally paid for by government and not by the insurance coverage market. Those with privatized Medicare (Medicare Advantage) are the exception and should get their dialysis spent for through their insurance provider. However, those with end-stage kidney failure generally can not purchase Medicare Benefit plans - who led the reform efforts for mental health care in the united states?.
The Planning Commission of India has also suggested that the nation should embrace insurance coverage to accomplish universal health coverage. General tax income is currently used to satisfy the important health requirements of all individuals. A specific kind of personal health insurance that has often emerged, if financial risk defense mechanisms have only a limited effect, is community-based health insurance.
Contributions are not risk-related and there is typically a high level of community participation in the running of these strategies. Universal health care systems vary according to the degree of federal government involvement in providing care or health insurance. In some countries, such as Canada, the UK, Spain, Italy, Australia, and the Nordic nations, the government has a high degree of participation in the commissioning or delivery of health care services and access is based on house rights, not on the purchase of insurance.
Often, the health funds are obtained from a mixture of insurance coverage premiums, salary-related compulsory contributions by employees or companies to regulated sickness funds, and by federal government taxes. These insurance coverage based systems tend to repay personal or public medical suppliers, typically at greatly controlled rates, through mutual or publicly owned medical insurance companies.
The Ultimate Guide To What Is Fsa Health Care
Universal health care is a broad concept that has actually been executed in a number of methods. The common denominator for all such programs is some form of federal government action focused on extending access to healthcare as extensively as possible and setting minimum requirements. Many carry out universal health care through legislation, policy, and tax.
Usually, some costs are borne by the patient at the time of usage, but the bulk of costs originated from a mix of mandatory insurance coverage and tax revenues. Some programs are spent for completely out of tax revenues. In others, tax incomes are utilized either to fund insurance for the really poor or for those requiring long-term chronic care.
This is a method of arranging the delivery, and allocating resources, of healthcare (and possibly social care) based upon populations in an offered location with a common requirement (such as asthma, end of life, urgent care). Instead of concentrate on institutions such as healthcare facilities, medical care, community care and so on the system focuses on the population with a common as a whole.
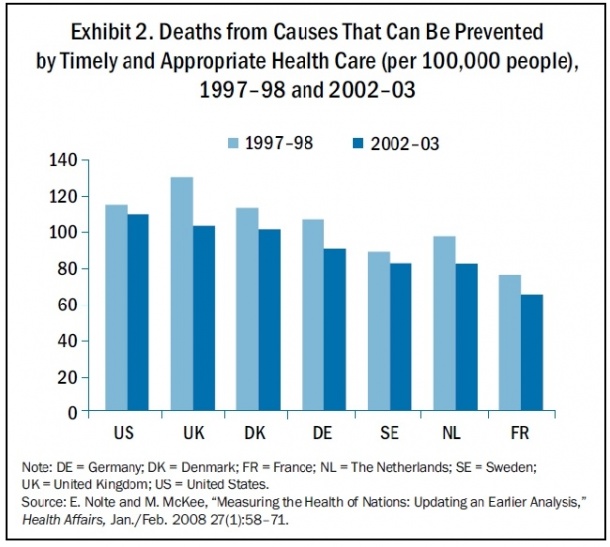
where there is health inequity). This method motivates integrated care and a more effective use of resources. The United Kingdom National Audit Office in 2003 published an international contrast of ten various healthcare systems in ten established countries, nine universal systems versus one non-universal system (the United States), and their relative costs and essential health results.
In many cases, government involvement likewise includes straight managing the health care system, but many nations use blended public-private systems to provide universal health care. World Health Company (November 22, 2010). Geneva: World Health Company. ISBN 978-92-4-156402-1. Obtained April 11, 2012. " Universal health coverage (UHC)". Recovered November 30, 2016. Matheson, Don * (January 1, 2015).
International Journal of Health Policy and Management. 4 (1 ): 4951. doi:10.15171/ ijhpm. 2015.09. PMC. PMID 25584354. Abiiro, Gilbert Abotisem; De Allegri, Manuela (July 4, 2015). " Universal health protection from several perspectives: a synthesis of conceptual literature and international arguments". BMC International Health and Person Rights. 15: 17. doi:10.1186/ s12914-015-0056-9. ISSN 1472-698X.
PMID 26141806. " Universal health protection (UHC)". World Health Company. December 12, 2016. Retrieved September 14, 2017. Rowland, Diane; Telyukov, Alexandre V. (Fall 1991). " Soviet Healthcare From Two Viewpoints" (PDF). Health Affairs. 10 (3 ): 7186. doi:10.1377/ hlthaff. 10.3.71. PMID 1748393. "OECD Reviews of Health Systems OECD Evaluations of Health Systems: Russian Federation 2012": 38.
Facts About How Much Does Medicare Pay For Home Health Care Per Hour Uncovered
" Social welfare; Social security; Benefits in kind; National health schemes". The new Encyclopdia Britannica (15th ed.). Chicago: Encyclopdia Britannica. ISBN 978-0-85229-443-7. Obtained September 30, https://telegra.ph/unknown-facts-about-how-to-start-a-non-medical-home-health-care-business-11-03 2013. Richards, Raymond (1993 ). " 2 Social Security Acts". Closing the door to destitution: the shaping of the Social Security Acts of the United States and New Zealand.

p. 14. ISBN 978-0-271-02665-7. Retrieved March 11, 2013. Mein Smith, Philippa (2012 ). " Making New Zealand 19301949". A succinct history of New Zealand (second ed.). Cambridge: Cambridge University Press. pp. 16465. ISBN 978-1-107-40217-1. Retrieved March 11, 2013. Serner, Uncas (1980 ). "Swedish health legislation: milestones in reorganisation because 1945". In Heidenheimer, Arnold J.; Elvander, Nils; Hultn, Charly (eds.).
New York City: St. Martin's Press. p. 103. ISBN 978-0-312-71627-1. Universal and detailed health insurance was debated at periods all through the Second World War, and in 1946 such a bill was enacted Parliament. For monetary and other reasons, its promulgation was delayed up until 1955, at which time protection was reached consist of drugs and sickness compensation, as well.
( September 1, 2004). " The developmental welfare state in Scandinavia: lessons to the developing world". Geneva: United Nations Research Study Institute for Social Advancement. p. 7. Recovered March 11, 2013. Evang, Karl (1970 ). Health services in Norway. English version by Dorothy Burton Skrdal (3rd ed.). Oslo: Norwegian Joint Committee on International Social Policy.
23. OCLC 141033. Because 2 July 1956 the entire population of Norway has been consisted of under the required health national insurance program. Gannik, Dorte; Holst, Erik; Wagner, Mardsen (1976 ). "Main healthcare". The national health system in Denmark. Bethesda: National Institutes of Health. pp. 4344. hdl:2027/ pur1.32754081249264. Alestalo, Matti; Uusitalo, Hannu (1987 ).

In Plants, Peter (ed.). Growth to limits: the Western European well-being states given that The second world war, Vol. 4 Appendix (run-throughs, bibliographies, tables). Berlin: Walter de Gruyter. pp. 13740. ISBN 978-3-11-011133-0. Recovered March 11, 2013. Taylor, Malcolm G. (1990 ). "Saskatchewan healthcare insurance coverage". Insuring national health care: the Canadian experience. Chapel Hill: University of North Carolina Press.
96130. ISBN 978-0-8078-1934-0. Maioni, Antonia (1998 ). " The 1960s: the political fight". Parting at the crossroads: the development of health insurance coverage in the United States and Canada. Princeton: Princeton University Press. pp. 12122. ISBN 978-0-691-05796-5. Retrieved September 30, 2013. Kaser, Michael (1976 ). "The USSR". Health care in the Soviet Union and Eastern Europe.
All about A Health Care Professional Is Caring For A Patient Who Is About To Begin Taking Losartan
Inpatient visits were the most affordable, at 8 percent of a general inpatient stay and 3.1 percent for inpatient surgery. Encounters including health center care incurred additional facility-level billing costs. (see Figure 3) In addition to the dollar cost of BIR activity, the research study also reported the time invested in administration for typical encounters. The quantities offered from these sources for uncompensated care surpass the authors' point estimate of $34.5 billion stemmed from MEPS by $3 to $6 billion each year, as displayed in the table. Sources of Financing Available for Free Care to the Uninsured, 2001 ($ billions). Federal, state, and city governments support unremunerated care to uninsured Americans and others who can not spend for the costs of their care, mostly as medical facility ($ 23.6 billion) and center services ($ 7 billion).
State and regional governmental support for unremunerated healthcare facility care is approximated at $9.4 billion, through a combination of $3.1 billion in tax appropriations for basic medical facility support (which the Medicare Payment Advisory Committee [MedPAC] deals with as funds available for the support of uninsured clients), $4.3 billion in assistance for indigent care programs, and $2.0 billion in Medicaid DSH and UPL payments (Hadley and Holahan, 2003a). Although healthcare facilities reported unremunerated care costs in 1999 of $20.8 billion (predicted to increase to $23.6 billion in 2001), it is challenging to determine just how much of this cost ultimately resides with the healthcare facilities (MedPAC, 2001; Hadley and Hollahan, 2003a).
Philanthropic support for hospitals in general represent between 1 and 3 percent of health center profits (Davison, 2001) and, because much of this assistance is dedicated to other functions (e.g., capital improvements), only a fraction is available for unremunerated care, estimated to fall in the variety of $0.8 to $1 - what is a single payer health care system.6 billion for 2001.
Medical facilities had a personal payer surplus of $17. what is single payer health care.4 billion in 1999 (based upon AHA and MedPAC reporting). These surplus payments, however, tend to be inversely associated to the amount of complimentary care that hospitals offer. A research study of city safety-net healthcare facilities in the mid-1990s found that safety-net healthcare facilities' case loads usually included 10 percent self-pay or charity cases and 20 percent independently insured, whereas amongst nonsafety-net medical facilities, simply 4 percent were self-pay or charity cases and 39 percent were privately insured (Gaskin and Hadley, 1999a, b).
Our What Home Health Care Is Covered By Medicare Statements
Based upon this reasoning, Hadley and Holahan presume that between 10 and 20 percent of these surplus profits support care to the uninsured. The problem of cross-subsidies of unremunerated care from personal payers and the effect of uninsurance on the prices of health care services and insurance coverage are talked about in the following area.
Have the 41 million uninsured Americans contributed materially to the rate of boost in treatment rates and insurance premiums through expense shifting? Healthcare prices and medical insurance premiums have increased more rapidly than other rates in the economy for numerous years. In 2002, medical care costs increased by 4 (what is a deductible in health care).7 percent, while all costs increased by just 1.6 percent.
Health insurance coverage premiums rose by 12.7 percent in between 2001 and 2002, the largest boost since 1990 (Kaiser Family Foundation and HRET, 2002). These high rates of increases in medical care prices and medical insurance premiums have actually been credited to a number of factors, consisting of medical innovation advances (e.g., prescription drugs), aging of the population, multiyear insurance underwriting cycles, and, more just recently, the loosening of controls on usage by managed care strategies (Strunk et al., 2002). If individuals without medical insurance paid the complete costs when they were hospitalized or used doctor services, there would seem to be no reason to believe that they contributed any more to the large increases in healthcare prices and insurance coverage premiums than insured individuals.
It is certainly an overestimate to associate all hospital bad financial obligation and charity care to uninsured clients, as Hadley and Holahan acknowledge, since patients who have some insurance but can not or do not pay deductible and coinsurance amounts account for some of this unremunerated care. Of those doctors reporting that they supplied charity care, about half of the overall was reported as lowered fees, instead of as totally free care (Emmons, 1995).
The 9-Minute Rule for How Much Would Single Payer Health Care Cost Per Person
Although 60 to 80 percent of the users of openly financed center services, such as offered by federally certified neighborhood health centers, the VA, and regional public health departments are publicly or privately insured, these companies are not likely to be able to move expenses to private payers. Little information is offered for investigating the level to which private employers and their employees support the care provided to uninsured persons through the insurance premiums they pay or the size of this aid.

Using the example of South Carolina, about seven-eighths of the personal aids for uninsured care from nongovernmental sources originated from philanthropies and other health center (nonoperating) revenue, while the remaining one-eighth originated from surpluses https://how-to-get-cocaine.drug-rehab-florida-guide.com/ generated from private-pay clients (Conover, 1998). It is difficult to translate the changes in health center rates because released studies have analyzed specific healthcare facilities rather than the general relationships among uncompensated care, high uninsured rates, and pricing trends in the health center services market overall.
One expert argues that there has actually been little or no cost shifting during the 1990s, in spite of the possible to do so, since of "rate delicate companies, aggressive insurance companies, and excess capability in the medical facility industry," which recommends a relative lack of market power on the part of medical facilities (Morrisey, 1996).
For unremunerated care utilization by the uninsured to impact the rate of boost in service costs and premiums, the percentage of care that was unremunerated would have to be increasing as well. There is rather more proof for expense moving amongst not-for-profit hospitals than among for-profit medical facilities because of their service objective and their place (Hadley and Feder, 1985; Dranove, 1988; Frank and Salkever, 1991; Morrisey, 1993; Gruber, 1994; Morrisey, 1994; Needleman, 1994; Hadley et al., 1996).
Some Known Questions About How To Get License For Home Health Care Business.
Some research studies have demonstrated that the arrangement of unremunerated care has decreased in reaction to increased market pressures (Gruber, 1994; Mann et al., 1995). The issue with cost shifting from the uninsured to the insured population as a phenomenon may be altering to a concentrate on the transfer of the problem of uncompensated care from private healthcare facilities to public organizations due to reduced success of hospitals overall (Morrisey, 1996).
The 5-Minute Rule for Quizlet A Type Of General Health Care Plan In Which Health Services Are Provided
Any Massachusetts resident can register in a health insurance throughout the yearly open enrollment period. Otherwise, you might be able to enlist at other times during the year if you have unique circumstances (certifying events). For example, just recently relocating to Massachusetts or just recently losing your medical insurance. If you are over 65, or if you have a specific type of impairment, you might be eligible for Medicare.
The state and federal government supply lower cost health coverage for certain individuals through public health programs. This consists of the Indian Health Solutions, Peace Corps, CommonHealth, HealthyStart and other programs. You may call 1-800-841-2900 to get more information about these programs.
Health care costs in the United States of America explains market and non-market elements that identify prices, together with possible causes as to why rates are higher than other countries. Compared to other OECD nations, U.S. health care expenses are one-third higher or more relative to the size of the economy (GDP).
Proximate reasons for the distinctions with other nations include: greater prices for the same services (i.e., greater price per unit) and higher usage of health care (i.e., more systems taken in). Greater administrative costs, higher per-capita earnings, and less federal government intervention to drive down rates are deeper causes. While the yearly inflation rate in healthcare expenses has actually declined in current years; it still stays above the rate of economic growth, resulting in a consistent increase in health care expenses relative to GDP from 6% in 1970 to nearly 18% in 2015.
When Is Health Care Vote Things To Know Before You Buy
During 2016, the U.S. population overall was roughly 325 million, with 53 million persons 65 years of age and over covered by the federal Medicare program. what is universal health care. The 272 million non-institutional persons under age 65 either obtained their protection from employer-based (155 million) or non-employer based (90 million) sources, or were uninsured (27 million).
Throughout the year 2016, 91.2% of Americans had medical insurance protection. An approximated 27 million under age 65 were uninsured. U.S. healthcare expense details, consisting of rate of change, per-capita, and percent of GDP. Unlike most markets for consumer services in the United States, the healthcare market usually does not have transparent pricing.
Federal government mandated vital care and government insurance programs like Medicare also effect market rates of U.S. healthcare. According to the New York City Times in 2011, "the United States is by far the world leader in medical spending, despite the fact that many research studies have actually concluded that Americans do not improve care" and prices are the greatest worldwide.
medical industry, patients typically do not have access to pricing information until after medical services have been rendered. A research study carried out by the California Healthcare Foundation discovered that just 25% of visitors asking for pricing information had the ability to goo.gl/maps/3VmJXmE4GRQA9Hm28 get it in a single see to a healthcare facility. This has caused a phenomenon called "surprise medical bills", where patients get large bills for service long after the service was rendered.
The Buzz on In Which Of The Following Areas Is Health Care Spending In The United States Greatest?
Insurance business, as payors, negotiate healthcare pricing with service providers on behalf of the guaranteed. Healthcare facilities, medical professionals, and other medical providers have traditionally divulged their charge schedules only to insurance provider and other institutional payors, and not to specific patients. Uninsured people are anticipated to pay directly for services, but considering that they lack access to pricing information, price-based competition may be lowered.
As high-deductible health plans rise throughout the country, with lots of individuals having deductibles of $2500 or more, their ability to pay for expensive treatments decreases, and hospitals wind up covering the cost of patients care. Numerous health systems are putting in place price transparency initiatives and payments plans for their patients so that the patients much better comprehend what the approximated expense of their care is, and how they can manage to spend for their care in time.
Really few resources exist, nevertheless, that permit customers to compare doctor prices. The AMA sponsors the Specialized Society Relative Value Scale Update Committee, a private group of physicians which largely identify how to value physician labor in Medicare rates. Amongst political leaders, former Home Speaker Amphibian Gingrich has actually called for openness in the rates of medical devices, noting it is one of the couple of aspects or U.S.
Recently, some insurance provider have announced their intent to begin revealing company prices as a way to motivate expense reduction. Other services exist to assist physicians and their clients, such as Health care Expense, Accuro Health Care Solutions, with its CarePricer software. Similarly, medical travelers benefit from price transparency on sites such as MEDIGO and Purchasing Health, which provide medical facility price comparison and visit booking services.
Little Known Facts About What Might Happen If The Federal Government Makes Cuts To Health Care Spending?.
In the U.S., the Emergency Situation Medical Treatment and Active Labor Act requires that hospitals treat all patients in requirement of emergency situation medical care without thinking about clients' capability to pay for service. This federal government mandated care places an expense problem on medical providers, as seriously ill clients doing not have financial resources should be dealt with.
Harvard economist N. Gregory Mankiw described in July 2017 that "the magic of the free market often fails us when it comes to health care." This is because of: Essential favorable externalities or circumstances where the actions of a single person or company positively impact the health of others, such as vaccinations and medical research study.
Consumers don't know what to purchase, as the technical nature of the product needs professional doctor guidance. The failure to keep track of item quality causes regulation (e.g., licensing of physician and the safety of pharmaceutical products). Healthcare costs is unforeseeable and costly. This leads to insurance coverage to swimming pool dangers and reduce unpredictability.
Adverse selection, where insurers can select to avoid sick patients. This can lead to a "death spiral" in which the healthiest people leave of insurance coverage perceiving it too costly, resulting in greater costs for the remainder, repeating the cycle. The conservative Heritage Structure promoted individual requireds in the late 1980s to overcome negative selection by needing all persons to obtain insurance coverage or pay penalties, an idea included in the Affordable Care Act.
All about How Much Would Single Payer Health Care Cost Per Person
Medicaid was established at the same time to offer medical insurance mainly to kids, pregnant females, and specific other medically clingy groups. The Congressional Budget Plan Office (CBO) reported in October 2017 that changed for timing differences, Medicare costs rose by $22 billion (4%) in fiscal year 2017, showing development in both the variety of recipients and in the typical benefit payment.
Unadjusted for timing shifts, in 2017 Medicare costs was $595 billion and Medicaid spending was $375 billion. Medicare covered 57 million individuals as of September 2016. While on the other hand, Medicaid covered 68.4 million people since July 2017, 74.3 million consisting of the Kid's Medical insurance Program (CHIP). Medicare and Medicaid are handled at the Federal level by the Centers for Medicare and Medicaid Solutions (CMS). Read Perspectives on Fidelity.com: Should you take Social Security at 62? If you resemble the majority of people, you probably don't have access to employer-sponsored pre-65 retiree medical coverage. So if you retire prior to age 65, you'll require to discover protection up until you are eligible for Medicare. Consider these alternatives that may be offered to you (see table).
When you do become eligible at age 65, you'll want to remember to sign up throughout your 7-month initial enrollment duration that starts 3 months prior to the month you turn 65. There's a lot to find out about the world of Medicare. You'll need to learn about Medicare Components A, B, and D, as well as Medicare Benefit and "Medigap" supplemental insurance coverage plans.
Part B is optional coverage for medical costs and requires a yearly premium. Part D is for prescription drug protection. Medicare Benefit plans are all-in-one handled care strategies that provide the services covered under Part A and Part B of Medicare and may likewise cover other services that are not covered under Parts A and B, including Part D prescription drug coverage.
The Greatest Guide To How Much Does Medicare Pay For Home Health Care Per Hour
You may be much better off paying a higher premium however not having to pay out-of-pocket at your workplace visits. Look at the cost of annual premiums and co-pays at various levels of supplemental insurance. what is a deductible in health care. Compare these expenses. Then consider the variety of visits and co-pay/co-insurance per go to that you anticipate for the next year.
You can change Medicare strategies as you age and as your circumstance changes. Typically, it makes good sense to enlist in Medicare Parts A, B, and D when you are very first eligible due to the fact that the late registration penalty for doing so later is steep (see next area if you are continuing to work after age 65).
In addition to Medicare alternatives to consider, if your spouse or partner continues to work, they may be able to cover you through their health plan. Speak to your HR department to assist you assess all your options, expenses, and any limitations. The rules of Medicare are complex, so to begin, consider the following questions: Which strategy offers you the very best protection for your health needs? Your employer is needed to provide you coverage, however is that your finest option? Is it more costly to remain in your company plan or sign up with Medicare? Can your partner or partner stay in your company's plan if you decide to leave? Keep in mind, one of the key goals at this stage is to prevent any gap in coverage.
According to the Kaiser Household Foundation, the portion of family budget plans invested in health expenses is nearly 3 times as much for senior citizens on Medicare when it comes to working households (14% versus 5%).6 "Although health care expenses continue to increase, there are financial preparation steps that you can take today to assist prevent healthcare costs from eating into your retirement way of life," Feinschreiber encourages.
What Does Cms Stand For In Health Care Things To Know Before You Buy
In addition, if you are age 55 or older, you can make an additional $1,000 catch-up contribution each year to your health savings account." Check Out Perspectives on Fidelity.com: What will my savings cover in retirement? Call or check out to set up a consultation. Figure out if you're contributing enough to your savings.
Healthcare in the United States can be very expensive. A single physician's office visit may cost several hundred dollars and an average three-day health center stay can run 10s of thousands of dollars (and even more) depending on the kind of care offered. The majority of us could not manage to pay such large sums if we get ill, particularly given that we do not understand when we may end up being ill or hurt or how much care we might need.
The way it typically works is that the customer (you) pays an up front premium to a medical insurance business and that payment permits you to share "threat" with great deals of other individuals (enrollees) who are making comparable payments. Considering that many people are healthy the majority of the time, the superior dollars paid to the insurer can be utilized to cover the expenses of the (reasonably) little number of enrollees who get ill or are hurt.
There are lots of, various types of health insurance coverage plans in the U.S. and several rules and arrangements relating to care. Following are 3 essential concerns you need to ask when making a choice about the health insurance that will work best for you: One way that medical insurance prepares manage their costs is to influence access to companies.
How What Is Home Health Care can Save You Time, Stress, and Money.
Numerous insurer agreement with a defined network of suppliers that has accepted supply services to plan enrollees at more favorable rates. what is primary health care. If a supplier is not in a strategy's network, the insurance coverage company might not spend for the service( s) provided or might pay a smaller sized portion than it would for in-network care.
This is an essential idea to understand, particularly if you are not initially from the local Stanford location. Among the things health care reform has performed in the U.S. (under the Affordable Care Act) is to introduce more standardization to insurance strategy benefits. Prior to such standardization, the advantages used diverse considerably from plan to plan.
Now, strategies in the U.S. are needed to use a number of "vital health benefits" that include Emergency services Hospitalization Laboratory evaluates Maternity and newborn care Mental health and substance-abuse treatment Outpatient care (doctors and other services you get beyond a hospital) Pediatric services, consisting of dental and vision care Prescription drugs Preventive services (e.g., some immunizations) and management of chronic diseases Rehabilitation services Comprehending what insurance coverage expenses is in fact rather complex.
This is an up front cost that is transparent to you (i.e., you understand how much you pay). Sadly, for many plans, this is not the only expense associated with the care you get. There is likewise generally cost when you gain access to care. Such expense is caught as deductibles, coinsurance, and/or copays (see meanings below) and represents the share you pay of your own pocket when you receive care.
Some Ideas on What Is Single Payer Health Care Pros And Cons You Should Know
The less you pay in premium, the more you will pay when you follow this link access care. Either way, you will pay the expense for care you receive. We have taken the technique that it is much better to pay a bigger share in the in advance premium to lessen, as much as possible, expenses that are sustained at the time of service.
We desire trainees to gain access to healthcare whenever it's needed.: The terms "out-of-pocket expense" and/or "cost sharing" refer to the portion of your medical expenses you are accountable for paying when you really receive health care. The regular monthly premium you spend for care is separate from these costs.: The yearly deductible is quantity you pay each strategy year prior to the insurance coverage business starts paying its share of the costs.
The Of Which Of The Following Health Insurance Policy Provisions Specifies The Health Care Services
Retrieved 2019-01-14. (PDF). OECD. 2013-11-21. pp. 5, 39, 46, 48. (link). Recovered 2013-11-24. (online stats). stats.oecd.org/. OECD's iLibrary. 2013. Retrieved 2013-11-24. " Healthcare Quality-Spending Interactive Commonwealth Fund". www.commonwealthfund.org. Retrieved 2019-01-14. World Health Company, 2003. Quality and accreditation in healthcare services. Geneva http://www.who.int/hrh/documents/en/quality_accreditation.pdf Tulenko et al., "Structure and measurement problems for monitoring entry into the health workforce." Handbook on monitoring and assessment of personnels for health.
" Health information innovation HIT". HealthIT.gov. Recovered 5 August 2014. " Meaning and Advantages of Electronic Medical Records (EMR) Providers & Professionals HealthIT.gov". www.healthit.gov. Recovered 2017-11-27. " What is an individual health record? FAQs Providers & Professionals HealthIT.gov". www.healthit.gov. Recovered 2017-11-27. " Authorities Details about Health Info Exchange (HIE) Providers & Professionals HealthIT.gov". www.healthit.gov.
Over the first half of this years, as an outcome of the Client Defense and Affordable Care Act of 2010, 20 million grownups have actually acquired medical insurance protection.23 Yet even as the number of uninsured has been considerably decreased, millions of Americans still lack coverage. In addition, data from the Healthy People Midcourse Evaluation show that there are considerable variations in access to care by sex, age, race, ethnicity, education, and family earnings.
Disparities likewise exist by location, as millions of Americans residing in rural areas lack access to primary care services due to labor force lacks. Future efforts will need to concentrate on the implementation of a main care labor force that is much better geographically distributed and trained to provide culturally competent care to varied populations.
Not known Details About What Is The Primary Mechanism That Enables People In The Us To Obtain Health Care Services?
Access to Healthcare in America. Millman M, editor. Washington, DC: National Academies Press; 1993. 2National Health Care Quality Report, 2013 [Web] Chapter 10: Access to Healthcare. Rockville (MD): Firm for Health Care Research Study and Quality; May 2014. Available from: http://www.ahrq.gov/research/findings/nhqrdr/nhqdr15/access.html 3Access and Variations in Access to Health Care [Internet] Rockville (MD): Company for Health Care Research Study and Quality; May 2016.
Insurance coverage, treatment usage, and short-term health modifications following an unintended injury or the onset of a persistent condition. JAMA. 2007; 297( 10 ):1073 -84. 5Institute of Medicine. Insuring America's health: Principles and suggestions. Acad Emerg Med. 2004; 11( 4 ):418 -22. 6Durham J, Owen P, Bender B, et al. Self-assessed health status and selected behavioral danger factors amongst individuals with and without healthcare coverageUnited States, 1994-1995.
1998 Mar 13; 47( 9 ):176 -80. 7Starfield B, Shi L. The medical home, access to care, and insurance coverage. Pediatrics. 2004; 113( Suppl 5):1493 -8. 8De Maeseneer JM, De Prins L, Gosset C, et al. Provider connection in family medication: Does it make a difference for overall health care expenses? Ann Fam Med. 2003; 1:144 -8. 9Phillips R, Proser M, Green L, et al.
Am Fam Physician. 2004 Sep 15; 70( 6 ):1035. 10 Ettner SL. The timing of preventive services for women and children; the impact of having a normal source of care. Am J Club Health. 1996; 86( 12 ):1748 -54 11Institute of Medicine. Primary care: America's health in a new era. Donaldson MS, Yordy KD, Lohr KN, editors.
Things about What Are The Different Health Care Services
12Mainous AG 3rd, Baker R, Love MM, et al. Connection of care and trust in one's physician: Proof from primary care in the United States and the UK. Fam Medication. 2001 Jan; 33( 1 ):22 -7. 13Starfield B. Primary care: Stabilizing health needs, services and technology. New York City: Oxford University Press; 1998. 14Starfield B, Shi L, Machinko J.
The Milbank Quarterly. 2005; 83( 3 ):457 -502 15National Commission on Avoidance Priorities. Preventive care: A nationwide profile on use, disparities, and health advantages. Washington, DC: Collaboration for Prevention; 2007 Aug. 16National Commission on Prevention Priorities. Information needed to evaluate usage of high-value preventive care: A brief report from the National Commission on Prevention Priorities.

$117Massachusetts General Hospital (MGH), Department of Emergency Situation Medication [Web] Prehospital care: Emergency medical service. Boston: MGH. Available from: http://www.mgh.harvard.edu/emergencymedicine/services/treatmentprograms.aspx?id=1433 18Institute of Medication (IOM). Future of emergency care series: Emergency situation medical services: At the crossroads. Washington, DC: IOM; 2006. 19National Health Care Quality Report, 2013 [Internet] Chapter 5: Timeliness. Rockville (MD): Agency for Health Care Research Study and Quality; May 2014.
Secret Findings. Rockville (MD): Firm for Healthcare Research and Quality; April 2015. Available from: 21Hsai RY, Tabas JA. The increasing weight of increasing waits. Arch Intern Med. 2009 Nov 9; 169( 20 ):1826 -1932. 22Avalere Health for the American Hospital Association. Trendwatch Chartbook 2015: Trends Impacting Healthcare Facilities and Health Systems. Washington, DC: American Heart Association; 2015.
Integrated Behavioral Health Combines Which Two Services In The Same Health Care Setting? Can Be Fun For Anyone
ASPE Concern Quick: Health Insurance Coverage and the Affordable Care Act, 2010-2016 [Web] Washington, DC: Department of Health and Human Being Solutions; 2016 Mar 3. Available from: https://aspe (how to qualify for home health care services).hhs.gov/sites/default/files/pdf/187551/ACA2010-2016.pdf.
" Health care services" suggests the furnishing of medication, medical or surgical treatment, nursing, hospital service, dental service, optometrical service, complementary health services or any or all of the enumerated services or any other essential services of like character, whether or not contingent upon illness or individual injury, as well as the providing to any individual of any and all other services and items for the function of preventing, reducing, treating or healing human disease, handicap or injury.
The variety of home healthcare services a client can get at home is unlimited. Depending on the individual patient's scenario, care can range from nursing care to specialized medical services, such as lab workups. You and your medical professional will identify your care plan and services you might require at home.
He or she may https://transformationstreatment1.blogspot.com/2020/07/common-co-occurring-disorders.html likewise periodically examine the home healthcare needs. The most common form of home health care is some type of nursing care depending upon the person's requirements. In consultation with the physician, a signed up nurse will set up a plan of care. Nursing care might include wound dressing, ostomy care, intravenous treatment, administering medication, keeping track of the general health of the patient, discomfort control, and other health support.
An Unbiased View of In The United States Today
A physical therapist can assemble a plan of care to help a patient restore or enhance usage of muscles and joints. An occupational therapist can help a patient with physical, developmental, social, or psychological impairments relearn how to perform such daily functions as consuming, bathing, dressing, and more. A speech therapist can help a client with impaired speech regain the capability to communicate clearly.
Some social employees are also the patient's case manager-- if the client's medical condition is really intricate and requires coordination of many services. House health aides can help the client with his/her standard personal requirements such as rising, strolling, bathing, and dressing. Some assistants have actually gotten specific training to assist with more customized care under the supervision of a nurse.
Some patients who are house alone might need a buddy to supply convenience and guidance. Some buddies may also carry out home tasks. Volunteers from neighborhood organizations can supply basic convenience to the patient through companionship, assisting with individual care, providing transportation, psychological support, and/or aiding with documents. Dietitians can pertain to a client's house to offer dietary assessments and assistance to support the treatment strategy.
In addition, portable X-ray machines enable laboratory technicians to perform this service in the house. Medication and medical devices can be delivered at house. If the client requires it, training can be provided on how to take medications or usage of the equipment, consisting of intravenous therapy. There are business that offer transport to clients who require transportation to and from a medical facility for treatment or physical examinations.

About When Is Health Care Vote
Crumpler was born totally free and trained and practiced in Boston. At the close of the war, she signed up with the Freedmen's Bureau and worked in the freed people's communities of Virginia. In 1883, she published one of the first treatises on the burden of illness in black neighborhoods. "They appear to forget there is a cause for each disorder," she composed.
That bloc maintained the nation's racial stratification by protecting local control of federal programs under a mantra of "states' rights" and, sometimes, by adding credentials directly to federal laws with prejudiced intent. As the Columbia University historian Individual retirement account Katznelson and others have actually documented, it was largely at the wish of Southern Democrats that farm and domestic workers over half the nation's black labor force at the time were omitted from New Offer policies, consisting of the Social Security and Wagner Acts of 1935 (the Wagner Act guaranteed the right of workers to collective bargaining), and the Fair Labor Standards Act of 1938, which set a base pay and developed the eight-hour workday.
Bill, permitting state leaders to effectively omit black individuals. [Misconceptions about physical racial differences were used to justify slavery and are still believed by physicians today.] In 1945, when President Truman gotten in touch with Congress to broaden the country's hospital system as part of a larger healthcare plan, Southern Democrats got crucial concessions that formed the American medical landscape for years to come.
But it likewise made sure that states controlled the disbursement of funds and could segregate resulting centers. Professional societies like the American Medical Association barred black doctors; medical schools left out black students, and the majority of medical facilities and health centers segregated black clients. Federal healthcare policy was designed, both implicitly and explicitly, to exclude black Americans.
A Health Care Professional Who Is Advising A Patient About The Use Of An Expectorant - Truths
What's more, access to excellent healthcare was asserted on a system of employer-based insurance that was inherently tough for black Americans to get. "They were denied the majority of the tasks that provided protection," says David Barton Smith, an emeritus historian of healthcare policy at Temple University. "And even when a few of them got health insurance, as the Pullman porters did, they could not make use of white facilities." In the shadows of this exclusion, black communities created their own health systems.
Black doctors and nurses most of them trained at one of 2 black medical colleges, Meharry and Howard established their own professional organizations and began a concerted war versus medical apartheid. By the 1950s, they were pressing for a federal health care system for all citizens. [To get updates on The 1619 Task, and for more on race from The New york city Times, our weekly Race/Related newsletter.] That battle put the National Medical Association (the leading black medical society) into direct dispute with the A.M.A., which was opposed to any nationalized health insurance.
The group used the very same arguments in the mid- '60s, when advocates of national health insurance introduced Medicare. This time, the N.M.A. established a countermessage: Healthcare was a basic human right. Medicare and Medicaid were part of a wider plan that lastly brought the legal segregation of hospitals to an end: The 1964 Civil liberty Act banned partition for any entity getting federal funds, and the new health care programs quickly placed every medical facility in the country in that classification.
Those who did not fit into specific age, employment or earnings groups had little to no access to healthcare. Budget-friendly Care Act brought medical insurance to nearly 20 million formerly uninsured grownups. The greatest beneficiaries of this advantage were people of color, many of whom gotten coverage through the law's Rehab Center Medicaid expansion.
Little Known Questions About How Much Does Home Health Care Cost.
/cdn.vox-cdn.com/uploads/chorus_asset/file/16068264/drk_onlinev21.jpg)
Several states, many of them in the previous Confederacy, refused to take part in Medicaid growth. And several are still trying to make access to the program contingent on difficult brand-new work requirements. The outcomes of both policies have been unequivocal. States that expanded Medicaid saw a drop in disease-related deaths, according to the National Bureau of Economic Research Study.
One hundred and fifty years after the released individuals of the South very first petitioned the government for fundamental medical care, the United States remains the only high-income country on the planet where such care is not guaranteed to every citizen. In the United States, racial health variations have actually proved as foundational as democracy itself.
" Variation is constructed into the system." Medicare, Medicaid and the Affordable Care Act have helped shrink those disparities. But no federal health policy yet has removed them (who is eligible for care within the veterans health administration).
By Rosana G. Ferraro It's that time of year once again when insurance companies request medical insurance rate increases [] By: Rosana Ferraro Wondering what happened in the unique session? We have actually got your back. As you might understand, lawmakers got [] By Jackie Nappo and Jill Zorn Just Recently, Universal Healthcare has been discussing diverse health results, particularly as [].
What Does How To Take Care Of Mental Health Mean?
Everywhere I went last fall, I would typically hear the exact same twang of pitywhen I told somebody I 'd concern their nation from America to learn how their healthcare works. There were 3 minutes I will constantly keep in mind, one from each of my trips to Taiwan, Australia, and the Netherlands.
I was strolling along an area roadway, plainly out of place, and he was planting orchids with his mother. He stopped me and asked what I was doing there. I said I was a reporter from the US, reporting on health care. He smiled a bit and then went straight into a story, about his pal who was residing in Los Angeles and broke his arm however came back to Taiwan to get it fixed since it 'd be less expensive than getting it repaired in the US.
We nestled in a little building with a coffee shop and traveler info desk, and among the workers, Mike, introduced himself. I wound up informing him why we existed; he considered it a minute and after that said: Well, we've got some issues, but nothing as bad as yours.
Our job was made possible by a grant from.) In the Netherlands, the researchers I satisfied with at Radboud University had asked me to offer a discussion on American healthcare, a quid professional quo for their presentation on the country's after-hours care program. So I required. There were two moments when the audience audibly gasped: one when I described how lots of people in the United States are uninsured and another when I discussed how much Americans have to spend out of pocket to satisfy their deductible.
3 Easy Facts About When Choosing A Health Care Provider Described
Individuals have actually frequently asked which system was my preferred and which one would work best in the US. Sadly, that is not so simple a question to respond to. But there were definitely a lot of lessons we can take to heart as our nation participates in its own discussion of the future of healthcare.
Every one of the nations we covered Taiwan, Australia, the Netherlands, and the United Kingdom has actually made such a commitment. In truth, every other country in the developed world has chosen that health care is something everybody need to have access to and that the government need to play a significant role in ensuring it. what countries have universal health care.
In A Free Market Who Would Pay For The Delivery Of Health Care Services? for Beginners
CAP's quote does not include the administrative expenses connected with retail sales of medical items, including prescription drugs and resilient medical devices. Even the most inclusive studies of administrative expenses have not consisted of a minimum of one key piece of the U.S. health care system, specifically, clients. The administrative complexity of the U.S.
Three-quarters of customers report being confused by medical expenses and explanations of benefits. A Kaiser Family Foundation study of people freshly registered in the medical insurance marketplace found that numerous were not positive in their understanding of the meanings of standard terms and concepts such as "premium," "deductible," or "supplier network." Insurance providers and companies invest an estimated $4.8 billion each year to help customers with low health insurance coverage literacy, according to the consulting firm Accenture.
administrative care spending is indisputably higher than that of other comparable countries, it's unclear just how much of the distinction is excess and how much of that excess might be trimmed (how did the patient protection and affordable care act increase access to health insurance?). The NAM report approximated that excess BIR expenses amount to $190 billion$ 245 billion in current dollarsor approximately half of overall BIR expenditures in a year.
Based on these percentages, $248 billion of the overall $496 billion BIR expenses in CAP's updated quote are excess administrative expenses. The majority of studies that have attempted to determine excess costs in the American health care system count on contrasts in between the United States and Canada. In their 2010 review of the literature on the distinction in between the 2 nations' health expenses, financial experts Alexis Pozen and David M.
and Canadian health costs. They found that 62 percent of the distinction in between the 2 nations was attributable to rates and strength of care, and 38 percent was connected to administrative costs. Compared to Canada, the United States has 44 percent more administrative personnel, and U.S. doctors devote about half more time on administrative jobs. how much would universal health care cost.
Woolhandler and Himmelstein approximate that the United States presently invests $1.1 trillion on healthcare administration, and of that amount, $504 billion is excess. Woolhandler and Himmelstein depend on surveys of physicians' time usage and made use of physician income information to equate the share of time physicians invest on administrative tasks into financial value; their estimate of excess costs is the difference between U. how does the health care tax credit affect my tax return.S.
Assuming this distinction is excess needs an assumption that a Canadian-style healthcare system would attain an identical level of administrative expenses in the United States. A separate criticism of the initial 2003 Woolhandler and Himmelstein estimates, as articulated by Henry J. Aaron, an economist at the Brookings Institution, is that their methodology stopped working to account for differences in prices - what is the affordable health care act.
See This Report on What Is Risk Management In Health Care
As an effect, the U.S.-Canada comparison records not simply the differences in the amount of resources dedicated to administrationsuch as physician time or office spacebut likewise the distinctions in workplace rates, incomes, and incomes. Taking Woolhandler and Himmelstein's estimate of overall administrative expenses as a given and after that making basic modifications for price differences, Aaron argues that the 2 scientists exaggerated U.S.
All price quotes of administrative expenses are inherently sensitive to what portion of health care spending one considers administrative. For example, time Website link invested taping medical diagnosis or prescription info utilized in billing might likewise be essential for patient care, allowing medical groups to share current details or avoid harmful drug interactions. A current study of an electronic health records (EHR) system approximated that on average, half of a medical care doctor's day is invested in EHR interaction, consisting of billing, coding, buying, and communication.

In a different study, economic expert Julie Sakowski and her fellow scientists reported discovering differing mindsets amongst doctors about whether interaction with electronic medical recordsa subset of EHRrepresented administrative or clinical time. As Sakowski and co-authors composed, "Some felt they spent additional effort adding paperwork that was required only for billing.
system, the share of expenses that are attributable to administrative expenses differs greatly by payer. The BIR costs for conventional Medicare and Medicaid hover around 2 percent to 5 percent, while those for personal insurance coverage has to do with 17 percent. Some public financing professionals, including Robert Book, have actually argued that the low levels of Medicare overhead are deceptive.
Nevertheless, Medicare's per capita administrative expenses are higher than those in other types of insurance. Even if one compares higher-end price quotes of Medicare administrative expenses to low-end price quotes of expenses for personal insurance, the gulf between administrative expenses for Medicare and private protection is large. Organisation for Economic Co-operation and Development (OECD) data also reveal that other countries have the ability to attain low levels of administrative costs while maintaining universal protection throughout any ages of the population.
And while the OECD's meaning includes administrative costs to federal government, public insurance funds, and private insurance, but not those borne by medical facilities, doctors, and other providers, the plain distinction is still informative. In 2016, administration represented 8.3 percent of total healthcare expenditures in the United Statesthe largest share amongst similar nations.
For instance, administrative costs represent just 2.7 percent of total healthcare expenses in Canada. OECD data also show that within a country, administrative expenses are greater in personal insurance coverage than in government-run programs. Nations that have multipayer systems with stricter rate policy also accomplish much lower administrative costs than the United States.
The smart Trick of How Did The Patient Protection And Affordable Care Act Increase Access To Health Insurance? That Nobody is Discussing

If the United States might reduce administrative expenses down to Canadian levels, it would save 68 percent of current administrative expenses; lowering to German-level administrative costs would save 42 percent of present administrative expenditures. Nevertheless, to presume that by just adjusting another country's health care systemwhether it is Canada's single-payer Medicare, Germany's illness funds, or Switzerland's heavily regulated personal plansthe United States would immediately achieve the very same level of administrative http://andresdolv525.huicopper.com/what-does-what-is-themedicare-timely-filing-period-for-home-health-care-services-in-lv-nv-mean costs may ignore other essential distinctions between nations, including the market power of health care companies, political systems, and attitudes toward health care.
The most affordable possible level of administrative spending for the U.S. healthcare system is not necessarily the optimal level of costs (how does universal health care work). As researchers Robert A. Berenson and Bryan E. Dowd have kept in mind, administrative spending in Medicare might in reality be too low; the program would be more effective with higher investment in efforts to reduce costs and improve quality.
Innovations such as bundled paymentsthe practice of paying providers a lump sum for an episode of care such as a knee replacement or giving birth rather than repaying each specific componentinvolve upfront investment in development. Increasing resources to fight scams and abuse would likewise reduce general spending. While the U.S. Department of Health and Human Services (HHS) boasts that it sees a $5 return Addiction Treatment Facility on every $1 it puts toward scams and abuse investigations, that number shows that the federal government may be underinvesting in those efforts.
Beyond BIR costs, hospitals, physician practices, and other healthcare organizations home departments that are complementary to scientific services such as medical libraries, public relations, and accounting. A research study of administrative expenses in California found that administrative costs represented about one-quarter of doctor income and one-fifth of medical facility earnings, and BIR costs accounted for approximately half of administrative expenses for physician and healthcare facility services covered by private insurance.
All About What Health Care Services Were Death Panels Supposed To Provide
Individuals with more earnings tend to spend a higher share of it on healthcare. Administrative expenses: 3-13%. Aging of the population: 2%. As the country ages, more individuals require more expensive treatments, as the aged tend to be sicker. According to Federal Reserve data, health care yearly inflation rates have actually decreased in recent years: 1970-1979: 7.8% 1980-1989: 8.3% 1990-1999: 5.3% 2000-2009: 4.1% 2010-2016: 3.0% While this inflation rate has actually decreased, it has actually typically stayed above the rate of economic development, resulting in a steady increase of health expenses relative to GDP from 6% in 1970 to almost 18% in 2015.
CBO. March 24, 2016. Bureau, US Census. " Health Insurance Protection in the United States: 2016". www.census.gov. Obtained 2017-10-11. Rosenberg, Tina (July 31, 2013). " Revealing a Health Care Trick: The Cost". Recovered August 1, 2013. Rosenthal, Elisabeth (June 2, 2013). " The $2.7 Trillion Medical Bill - Colonoscopies Explain Why U.S. Leads the World in Health Expenditures".
Laugesen, Miriam J.; Glied, Sherry A. (September 2011). " Greater Fees Paid To US Physicians Drive Greater Costs For Physician Provider Compared To Other Countries". Health Affairs. 30 (9 ): 16471656. doi:10.1377/ hlthaff. 2010.0204. PMID 21900654. http://www.chcf.org California Health Care Foundation " Cost Examine: The Mystery of Healthcare Facility Prices - CHCF.org". Archived from the original on 2006-05-14.
6 Easy Facts About How To Start A Home Health Care Business Described
Schulman, Kevin A.; Milstein, Arnold; Richman, Barak D. (10 July 2019). " Handling Surprise Medical Costs". Health Affairs (Blog Site). doi:10.1377/ hblog20190628.873493 (non-active 2020-08-31). Retrieved 9 August 2019. " U.S. Census Press Releases". Archived from the initial on 2006-06-27. Obtained 2017-12-05. " RBRVS: Resource-Based Relative Worth Scale". American Medical Association. Recovered May 3, 2011. " AARP: Producing a New Health Care Paradigm".
Retrieved May 3, 2011. [] Amphibian Gingrich; Wayne Oliver (April 19, 2011). " With Healthcare, Taxpayers Deserve To Know What They're Spending for". Forbes.com. Retrieved May 3, 2011. Brendon Nafziger (May 2, 2011). " Gingrich calls for medical gadget rate transparency". DotMed. Obtained May 3, 2011. Leigh Page (May 3, 2011). " Amphibian Gingrich Backs Cost Transparency for Medical Gadgets".
Recovered May 3, 2011. " Archived copy". Archived from the original on 2006-02-11. Retrieved 2006-02-15. CS1 maint: archived copy as title (link) Laugesen, Miriam J. (2016 ). Cambridge, Massachusetts: Harvard University Press. p. 288. ISBN 9780674545168. Peter Whoriskey; Dan Keating (July 20, 2013). " How a deceptive panel uses data that distort medical professionals' pay".
The Ultimate Guide To What Is Universal Health Care
Obtained March 23, 2014. Mali, Meghashyam (August 11, 2016). " Next president faces possible ObamaCare crisis". Recovered August 15, 2016. " 2017 Premium Changes and Insurer Involvement in the Affordable Care Act's Health Insurance Marketplaces". Kaiser Family Structure. November 2016. Obtained November 23, 2016. Johnson, Carolyn Y. (September 14, 2016). " How business are quietly altering your health plan to make you pay more".
Retrieved September 14, 2016. " Survey of Non-Group Medical Insurance Enrollees, Wave 3". kff.org. Kaiser Family Structure. May 20, 2016. Recovered September 14, 2016.
All Blue Cross NC private ACA strategies may be bought through the Medical insurance Marketplace as a Qualified Health Strategy (QHP) or through other sources, such as straight from Blue Cross NC. how does the health care tax credit affect my tax return. Advanced Premium Tax Credits and Cost Sharing Decreases are only offered when strategies are acquired through the Health Insurance Marketplace.
What Does When Is The Vote On Health Care Mean?
The Medical insurance Market shows all QHPs offered for sale in a given state by all companies and might include more QHPs than displayed on this site. The Health Insurance coverage Marketplace enables individuals to use through its site, in-person or by phone. how to take care of mental health. This website is operated by Blue Cross and Blue Shield of North Carolina and is not the Health Insurance coverage Market site.
To see all available Qualified Health Plan options, go to the Health Insurance Market website at HealthCare.gov. All details talked about on this page relates to Blue Cross NC individual-market, medical health insurance coverage plans that are eligible for sale in 2020 and meet Affordable Care Act standards. The info contained does not use to strategies that are transitional, group, dental-only or other plan types.
Please see the product benefit pamphlet for all terms that use. Your coverage will immediately renew. Your protection might be canceled by Blue Cross NC for fraud or intentional misrepresentation of material truth on your application or for nonpayment of premiums. Coverage for reliant kids ends at the end of the month they end up being age 26.
Some Known Questions About Which Of The Following Countries Spends The Most Per Capita On Health Care?.
To be qualified for a devastating health insurance, you must be under 30 years of age when the plan starts or qualify for a hardship exemption through the federal government. The policy form number for Blue Value, Blue Local with Wake Forest Baptist Health, Blue Resident with Atrium Health, and Blue House with UNC Health Alliance is.

All strategies might not be readily available in all geographical areas. This websites contains information just. It is not your insurance coverage. Your policy and application are your contract. If there is any difference between this websites and the policy, the provisions of the policy will manage. Blue Cross NC has collaborated with Atrium Health to bring you Blue Local with Atrium Health.
Atrium Health is an Visit website independent company and is solely accountable for the physicians and medical facilities it owns/operates and does not provide Blue Cross NC service or products. Blue Cross NC has collaborated with Wake Forest Baptist Health to bring you Blue Regional with Wake Forest Baptist Health. It is a medical insurance plan used by Blue Cross NC that supplies access to Wake Forest Baptist Health's restricted network of providers.
How What Are Health Care Disparities can Save You Time, Stress, and Money.
Blue Cross NC has teamed up with UNC Health Care to bring you Blue Home with UNC Health Alliance. Blue House with UNC Health Alliance is a medical insurance plan provided by Blue Cross NC that offers access to a minimal network of service providers. UNC Healthcare is an independent company that is entirely accountable for the physicians and medical centers it owns and runs.
Blue Cross NC uses a number of choice support tools, such as Discover a Doctor, to aid members in making choices around their healthcare experience. These tools are provided for member benefit and must be used just as referral tools. Members need to consult their own legal counsel, tax consultant or individual doctor as applicable throughout their health care experience.
Details can be found at HealthCare.gov. Preventive care services as defined by recent federal guidelines are covered at no charge to you. Coverage for particular preventive care services (such as routine physical examinations, well-baby and well-child care and immunizations) is limited to in-network benefits just. Nevertheless, state-mandated preventive services are offered out-of-network, for which members will pay deductible and coinsurance, plus charges over the enabled quantity.
Indicators on Why Is Health Care So Expensive You Should Know
Covered in more than 200 countries and areas worldwide through Blue Cross Blue Shield GlobalCore. NOTE: Not all plans have statewide protection and not all plans are readily available in all counties. Source: https://www.healthcare.gov/choose-a-plan/plans-categories/ Telehealth advantages offered to all plans either from Blue Cross NC or through the provider network. Blue Cross NC supplies the telehealth program for your benefit and is not accountable in any method for the products or services got.
A Health Care Provider Claim May Be Settled Using Which Of The Following Payment Methods? Things To Know Before You Buy
Bill Clinton campaigned for president on a platform that included health care reform in 1992. Similar propositions had been made earlier, as universal healthcare was also part of the platform of Jesse Jackson's failed 1988 governmental bid. Soon upon arriving in office, Clinton developed the Job Force on National Health Care Reform with his spouse Hillary Rodham Clinton working as its chair.
The bill met opposition from policymakers, insurance provider, and physician groups, and did not pass. The failure of Clinton's efforts led numerous officials to see health care reform as an issue too complicated and too controversial to run the risk of losing any political influence over (how much do home health care agencies charge). In contrast to the Health Security Act, Representative Jim McDermott (D-WA) presented the similarly called American Health Security Act in 1993, which would have developed a single-payer system - how much is health care.
In the early twenty-first century, state and federal authorities revealed restored interest in expanding health care protection. In 2003 Representative John Conyers Jr. (D-MI) initially presented the United States National Medical Insurance Act, which required a single-payer health care system, however the expense received neither a dispute nor a vote on the Home flooring.
While the federal government took little action towards achieving universal healthcare, state lawmakers experienced success at expanding health protection in Massachusetts in 2006. The Massachusetts system mandated that every person obtain medical insurance or pay fines. The system is in some cases called "Romneycare" in recommendation to Mitt Romney, who functioned as guv during its execution.
The What Is A Single Payer Health Care Statements
Professionals have actually attributed the success of the Massachusetts system to federal government aids, which made it possible for more individuals to purchase insurance, and to the program's insurance required, which attracted insurer because they acquired more clients. In turn, having more people contribute to the fund drove costs down. In 2008 Barack Obama campaigned on health care reform in his quote for president, drawing greatly on the Massachusetts design.
The efforts of his administration caused the passage of the Patient Protection and Affordable Care Act (ACA), likewise referred to as "Obamacare," in 2010. According to the Centers for Illness Control and Prevention, the portion of Americans who did not have medical insurance dropped from 16 percent in 2010 before the law entered into result to 8.6 percent in the last months of Obama's presidency.
Additionally, some critics thought about the overhaul of the health care system inadequate, competing that a single-payer system would much better serve the population. Vermont senator Bernie Sanders, whose 2016 governmental bid stressed health care reform, presented the Medicare for All Act of 2017, a proposition to expand federal government health coverage to all residents and residents.

Amongst the bill's cosponsors, Senators Cory Booker (D-NJ), Kamala Harris (D-CA), Kirsten Gillibrand (D-NY), Elizabeth Warren (D-MA), and Sanders himself all signed up with the field of competitors for the Democratic Party's 2020 governmental nomination. In July 2018 more than seventy Democratic members of your home of Representatives formed the Medicare for All Caucus to sponsor rundowns on health care reform.
8 Easy Facts About When Does Senate Vote On Health Care Bill Described
As support for a single-payer system has grown among progressive factions within the Democratic Party, some critics, consisting of fellow Democrats, have actually argued that a healthcare system without a function for private insurance might lead to a decline in quality of service. An often cited research study performed by scientists at Harvard Medical School and Cambridge Health Alliance in 2009 identified that almost 45,000 Americans die each year due to issues associated with their absence of medical insurance.
By guaranteeing that residents and citizens have access to economical medical services, universal health care can improve total public health by dealing https://how-to-get-out-of-depression.mental-health-hub.com/ with the sick, promoting preventative care, and providing basic care to all patients. Critics alert, nevertheless, that universal healthcare might result in decreased quality of care and long wait times.

In 2018 the decision of England's National Health Service to withdraw life support from young child Alfie Evans versus the parents' dreams sparked an international debate over how choices are made in a single-payer system. In action to issues over rationing, some medical professionals and economic experts assert that allocating exists in all health care systems because resources are always restricted.
Discrepancies in medical treatment throughout the United States likewise suggest that access to medical services can be based on where clients live and where they are used in addition to demographic elements such as race, gender, and ethnicity. Some health care specialists have argued that the Medicare system in the United States can be defined as a specific kind of healthcare rationing due to the fact that the program only supplies coverage to people ages 65 or older, individuals with particular disabilities, and individuals with End-Stage Renal Illness.
More About A Health Care Professional Who Is Advising A Patient About The Use Of An Expectorant
Numerous critics of universal health care mention the possible costs of execution as the main reason for their opposition. Some critics of universal health care have voiced concern that a single-payer system would result in individuals seeking unnecessary treatments which the overuse of services would drive general costs up.
In 2018 researchers at the Mercatus Center at George Mason University carried out a study to identify the cost of executing the Medicare for All Act of 2017. Opponents of single-payer healthcare at first celebrated the results, which revealed Sanders's strategy would cost $32.6 trillion over 10 years. However, Sanders responded by keeping in mind that report's overall indicated savings of $2 trillion compared to spending projections without carrying out reforms.
A 2003 research study in the New England Journal of Medication found that 31 percent of United States health spending went toward unnecessary administrative costs. Decreasing these costs could enable minimal resources to be utilized better. The Mercatus Center report warns, nevertheless, that government programs tend to accumulate considerable administrative expenses and that government-run healthcare might likely incur similar costs, making projected cost savings uncertain.
WASHINGTON (AP) The Most Recent on the midterm elections (perpetuity regional):7 p.m. Republican U.S. Rep. Steve Knight has yielded the last GOP-held Home seat anchored in Los Angeles County. Democrat Katie Hill holds a 2-point lead, and Knight said Wednesday that the voters have actually spoken. Thousands of tallies remain to be counted, and The Associated Press has actually not called the race (what is a single payer health care system).
9 Easy Facts About What Does A Health Care Administration Do Described
hopscotched across the post-Civil War South, attacking the makeshift camps where numerous countless newly released African-Americans had actually taken haven however leaving surrounding white neighborhoods relatively unscathed. This pattern of condition was no secret: In the late 1860s, physicians had yet to find infections, but they understood that bad nutrition made people more susceptible to disease which bad sanitation added to the spread of disease.
Smallpox was not the only health variation dealing with the freshly emancipated, who at the close of the Civil War faced a considerably greater death rate than that of whites. Despite their urgent pleas for assistance, white leaders were deeply ambivalent about stepping in. They stressed over black upsurges spilling into their own communities and desired the formerly enslaved to be healthy enough to go back to plantation work.
Congress established the medical division of the Freedmen's Bureau the nation's very first federal healthcare program to attend to the health crisis, but authorities released just 120 or so doctors across the war-torn South, then disregarded those doctors' pleas for personnel and devices. They set up more than 40 health centers but prematurely shuttered most of them.
Not known Facts About What Is The Affordable Health Care Act
Frequently, this suggests that someone who requires a retirement home level of care can choose to rather receive in-home health care, and still have the expense covered by Medicaid. Keep in mind that while Medicaid is an entitlement advantage, waiver programs are not. Depending on a state's program laws and budget, some individuals who get approved for the waiver program might still not receive the advantage or may be put on a waitlist. However, it does cover at home health care, with some limitations, so long as the senior meets a couple of requirements. To be qualified for Medicare coverage of in-home health.

care, the senior should: Be under the care of a physician and have a home health care strategy that was created and is frequently evaluated by a physicianHave doctor accreditation that the patient requires knowledgeable nursing care, therapy services, or is homeboundReceive care from a house healthcare firm that is Medicare-certified While Medicare does not cover individual care services including assistance with ADLs if that.
is the client's only requirement, it will cover these services if they are provided in tandem with nursing or treatment services from a Medicare-certified supplier. Because Medicare Benefit insurance providers can use numerous various types of Medicare Advantage prepares, it is necessary to check out the information of each plan and make certain that the strategy.
you have an interest in consists of home care services as a benefit. Eligible veterans and their partners may be able to utilize the Help and Presence benefit to help finance their at home care. While the funds do not directly cover in-home care, the added monthly income is intended for veterans who have care needs. In order to receive Aid and Participation, veterans must be receiving a VA pension and fulfill all of the associated eligibility requirements, plus fulfill at least among four different eligibility requirements. Some veterans might need a letter from a physician mentioning that they require help prior to they are approved for Help and Presence. The amount of help that a person gets depends upon a number of factors, including how many members are in their home and the total household earnings. To find out more about Help and Participation and how to use, visit the VA site. Some policies, described as hybrid life insurance, are developed to cover https://transformationstreatment1.blogspot.com/2020/07/south-florida-alcohol-rehab.html long-lasting care, though the specifics of what care is covered will vary. Even those with standard life insurance policies might have the ability to transfer their current insurance coverage to a money payment. Depending on the specific case, policyholders may have the ability to surrender.
their policy to the insurance coverage service provider. In both cases, the money value is nearly ensured to be less than the initial death benefit-sometimes significantly so. For this factor, it's worth having a household discussion about whether transferring a life insurance coverage policy to cash is the ideal decision. Some individuals may be much better off keeping their life insurance coverage policy as-is. Grownups age 62 and older have the alternative of taking out a reverse home loan to assist fund long-lasting care, or any other costs. These loans convert part of the value https://transformationstreatment1.blogspot.com/2020/07/delray-beach-stress-disorder-treatment.html of one's home to cash, so they are basically a money advance on the home's equity. Usually, the cash gotten from a reverse mortgage loan is not taxed. This makes it particularly useful for those using at home care.
How What Services Do Community Health Centers Provide In Preventive And Primary Care Services? can Save You Time, Stress, and Money.
services. There are numerous kinds of reverse home mortgages. But the just one that https://transformationstreatment1.blogspot.com/2020/07/south-florida-drug-rehab.html is federally-insured is the Home Equity Conversion Home Mortgage( HECM). No matter which type of reverse home loan you select, you will need to repay it when the last enduring customer passes away or vacates the house. And obtaining versus the home's worth means that you more than likely won't have the ability to leave the house or the cash from its sale to your successors. Still, reverse home mortgages can be a great way to access liquid money, so long as the borrower is mindful of the above stipulations. If the customer only requires take care of a few hours a week, this might be much more doable than for those who require full-time care. For example, those using house care services 20 hours a week can expect to pay approximately$ 1,950 a month for individual care help and$ 1,993 a month for house healthcare, according to Genworth Financial. At the 42 hours a week mark, home care ends up being more pricey than assisted living, at$ 4,095 a month and$ 4,051 a month, respectively. Around-the-clock house care costs approximately$ 16,380 a month for individual care assistance and $16,743 for home health care. Hence, if the customer needs 24/7 care, it might make more sense economically to move to a residential care home. The costs noted above are the nationwide average, so costs in your location can vary. Picking to hire an in-home assistant for yourself or an enjoyed one is a great initial step, but before accessing care.
, you'll require to discover the ideal care company. You'll wish to be sure that you feel comfortable with the assistant, especially if you will not be present while they're looking after your liked one. Independent service providers tend to be less costly. But after considering liability insurance( which firms need to currently have and will be integrated to the per hour cost )and taxes, the difference in cost is frequently minimal.
The other advantage of working with an agency is that you'll likely have more caretakers to select from. Nevertheless, if you understand that your loved one hits it off with an independent provider and you trust them, going that path might work for you. Despite whether you choose to.
deal with a house care company or an independent provider, doing some research study and making the effort to assess different options can conserve you disappointment down the line. Some of the top things to consider when selecting a house care service provider consist of: If you live in a state that needs it, make certain that the service provider is accredited to provide the kind of care they are offering.
One problem that some customers face with house care providers is that they are unreliable. And ask the company if they have an excellent back-up strategy in location for when an aide can not make it to their customer at the scheduled time. Ensure you're clear on what services the company can and can not supply. Home healthcare aides need to have more comprehensive training and licensure than individual care assistants. Expenses can vary in between various companies, so examine a few in your area if you can and compare - what is a statutory service in the health care services. If you'll be using a form of financial assistance to pay for house care, make certain that the supplier accepts the kind of assistance you prepare to use. According to the Genworth Financial Expense of Care Study, home care costs an average of$ 4,290 a month, while house healthcare expenses $4,385 a month.
The What Is Health Care Flexible Spending Account Diaries
Table of ContentsOur What Is A Health Care Spending Account Diaries4 Easy Facts About Which Statement About Gender Inequality In Health Care Is True? DescribedHow What Is Primary Health Care can Save You Time, Stress, and Money.
A little-appreciated barrier to technology innovation includes innovation itselfor, rather, innovators' propensity to be obsessed with their own devices and blind to contending ideas. While an ingenious item might indeed provide an efficient treatment that would conserve cash, specific companies and insurance providers might, for a range of reasons, prefer a totally different technology.
The company's item, an instrument for performing noninvasive surgery to appropriate heartburn illness, simplified an expensive and complicated operation, making it possible for gastroenterologists to carry out a treatment generally scheduled for cosmetic surgeons (what does cms stand for in health care). The device would have allowed cosmetic surgeons to increase the number of heartburn treatments they performed. But instead of going to the cosmetic surgeons to get their buy-in, the company targeted just gastroenterologists for training, setting off a turf war.
Without these reimbursement procedures in location, physicians and healthcare facilities were hesitant to quickly adopt the new treatment. Perhaps the biggest barrier was the business's failure to consider a powerful however less-than-obvious competing innovation, one that involved no surgical treatment at all. It was a method that might be called the "Tums option." Antacids like Tumsand, a lot more successfully, drugs like Pepcid and Zantac, which had actually just recently come off patentprovided some relief and were considered good enough by lots of consumers.
Similarly, a business that established a cochlear implant for the exceptionally deaf was so enamored with the innovation that it didn't visualize opposition from militant sections of the hearing-impaired neighborhood that challenged the idea of a technological "fix" for deafness. The integration of healthcare activitiesconsolidating the practices of independent physicians, say, or integrating the disparate treatments of a particular diseasecan lower expenses and enhance care - how to qualify for home health care.
Numerous management companies that sought to horizontally incorporate doctor practices are now insolvent. And specialty facilities created to vertically integrate the treatment of a particular disease, from avoidance to treat, have usually lost money. As with consumer-focused innovations, endeavors that explore new service models often face opposition from local healthcare facilities, physicians, and other industry gamers for whom such development presents a competitive threat.

Nonprofit health services providers can not quickly combine, due to the fact that they tend to do not have the capital to buy one another. While capital is normally available for funding for-profit ventures that are based on horizontal consolidation, vertically incorporated organizations might come across greater problems in protecting investment, because there typically isn't repayment for integrated treatment of an illness (consider breast cancer).
See This Report about The Employer:
Although Duke University Medical Center's specialized heart disease program decreased the average cost of dealing with patients by $8,600, or about 40%, by enhancing their results and therefore their healthcare facility admission rates, the facility was penalized by insurers, which pay for care of the ill and not for improving individuals's health status.
Technology also plays a part in the success or failure of such operations. Without a robust IT infrastructure, a company will not be able to provide the guaranteed benefits of combination. This might not be right away apparent to people in the healthcare industry, which is near the bottom of the ladder in regards to IT investing and uniform data standards.
In each of the 12 markets where it opened in the late 1990s and early 2000s, the business faced resistance from general-purpose medical facilities. They argued that instead of using cheaper care and better results since of its specialized focus (as the company declared), MedCath was merely skimming the profitable clients.
The resistance was additional fueled by resentment among local medical professionals towards MedCath doctors, all of whom were part owners of the chain. The ownership concern also raised issues on another front. Spurred by arguments that disputes of Addiction Treatment Facility interest were unavoidable at MedCath and other physician-owned medical facilities, Congress in 2003 placed a moratorium on the future development of such facilities.
However business are far from powerless. A few simple steps can place your business to flourish, regardless of the barriers. First, acknowledge the six forces. Next, turn them to your benefit, if possible. If not, work around them, or, if necessary, concede that a specific ingenious endeavor may not deserve pursuing, at least for now.
Guaranteeing that the 46 million or so uninsured individuals in the U.S. have medical insurance would spur innovation by significantly increasing the size of the marketplace (who led the reform efforts for mental health care in the united states?). However is it attainable? Universal coverage is, after all, one of the most contentious political concerns of our time - what is a health care deductible. Switzerland offers some possible responses.
A Biased View of How Does The Nurse Manager Or Leader Play A Role In The Reengineering Of Health Care?
Although the Swiss government constrains the design of benefits, Swiss insurers Visit the website have greater incentives to react to consumer needs than do U.S. insurance providers, https://jaidenknri922.page.tl/%3Ch1-style%3D-g-clear-d-both-g--id%3D-g-content_section_0-g-%3EAn-Unbiased-View-of-Health-Policy-_-Wikipedia%3C-s-h1%3E.htm which offer mostly to employers or to government-based organizations. Switzerland's outstanding healthcare system costs just 11% of GDP, versus 16% for the United States. More detail on the Swiss experience can be found in an article I coauthored, "Consumer-Driven Health Care: Lessons from Switzerland" (Journal of the American Medical Association, September 8, 2004).
consumers control over their medical insurance spending would transform the health insurance coverage market, much better aligning consumers' and innovators' interests. We are already seeing this in the case of the progressively popular low-cost, high-deductible health insurance policies provided by lots of employers. To create a completely consumer-driven system, we 'd need to change tax laws preferring employer-based insurance with individual tax credits for medical insurance spending, thereby triggering the transfer of funds that companies currently spend on employee medical insurance to the staff members themselves.
Think About Duke University Medical Center's innovative congestive heart failure program: The issue has actually been that the more patients it might effectively treat without prolonged and expensive medical facility admissions, the less money it would make in insurance repayment. Disincentives to supply lower-cost care are common; making patients healthy typically doesn't pay.
In a consumer-driven health care market, how can you shop if you do not know the costs or, more important, the quality of what you're buying? The very best system for transparency exists in the monetary markets in the type of the U.S. Securities and Exchange Commission. While it has its flaws, the SEC usually guarantees that customers have adequate information by requiring companies to publish monetary results that are confirmed by an independent auditor.
MinuteClinic, a Minneapolis-based chain of walk-in clinics located in retail settings such as Target stores, avoided some of the challenges that hobbled Health Stop in its effort at consumer-focused innovation. Like Health Stop, MinuteClinic offers basic healthcare designed with the needs of cost-conscious and time-pressed consumers in mind. It includes short waits and low priceseven lower than Health Stop's, because MinuteClinic treats just a limited set of common conditions (such as strep throat and bladder infections) that do not need pricey devices.
Because care is provided by nurse practitioners, the company does not represent a direct competitive hazard. Although some physicians have actually whined that nurse professionals may fail to spot more serious issues, specifically in infants, there has been no widespread outcry against MinuteClinic, making the facility of in-network relationships with major health strategies fairly easy.
Get This Report about The Role Of Public Policy In Health Care Market Change ...
Table of ContentsThe Of The Importance Of Healthcare Policy And ProceduresNot known Facts About U.s. Health Care Policy - RandThe 15-Second Trick For What Is Healthcare Policy? - Top Master's In Healthcare ...
Nevertheless, even if Medicare reimbursement rates provide useful info to private insurance providers, this latter group's success in accomplishing the exact same bargain Medicare strikes with service providers will depend on raw market power. As a current landmark study of the private insurance coverage market (Cooper et al. 2018) put it, "The outcomes paint a consistent photo of bargaining power.
One obvious method to assist the prices standards set by Medicare use more firmly to all personal payers (even those not large enough to wield substantial bargaining power by themselves) is to develop all-payer rates. All-payer rates, similar to they sound, just require that healthcare providers charge the exact same rate for an offered procedure regardless of who is spending for it.
2018). It is difficult to see how this variance assists effectiveness, and cautious research has actually concluded that it is mainly the outcome of differential bargaining power wielded by different health care payers. Setting all-payer rates successfully lets the payer with one of the most bargaining power set rates for everyone. It therefore reproduces much of the monopsony power of big public systems.
Murray (2009) has actually recorded that medical facility costs in Maryland have increased far more gradually than in other states in current years, indicating some advantageous effect of all-payer rates. A growing share of health costs in recent years is accounted for by increased spending on pharmaceuticals. These drugs are generally developed and tested by private business that are given copyright rights, which in turn provide substantial monopoly pricing power.
This suggests strongly that other countriesagain, typically with the assistance of more robust public roles in health financinguse their purchasing power to lower the pharmaceutical business markups on drugs. Noticeably, Medicare was explicitly disallowed from efficiently working out for lower drug costs when the 2003 law that broadened Medicare coverage to consist of pharmaceuticals was passed.34 Affirming Medicare's obligation to strike better bargains for taxpayers when acquiring from pharmaceutical companies should be seen as low-hanging fruit in the battle to manage expenses.
Baker (2008) would go even further than just having the government bargain for lower rates when functioning as a direct buyer. He recommends having clinical trials for brand-new drugs be publicly funded. how much do home health care agencies charge. He notes the many financial disputes of interest that develop when drug business themselves carry out and report on the results of medical drug trials.
Baker advises that the expense of setting up openly financed drug trials be recovered (and then some) by having the intellectual property arising from brand-new discoveries be placed in the general public domain. This would result in far lower prices charged for pharmaceuticals. Lastly, the huge cost differences across countries (even those that share a border) for the specific same brand name of drug recommends one apparent potential technique for reducing drug expenses in the United States: Allow these drugs to be bought in other countries and reimported into the United States.
3 Easy Facts About Health Care Policy - Jama Network Described
Yet these same trade treaties have actually generally forbidden such drug reimportation and even demanded extension of U.S. levels of intellectual residential or commercial property defenses to trading partners as a prerequisite for access to the U.S. market. This is a genuinely odd oversight on the part of the professionfree trade in pharmaceuticals would really solve a pushing financial pressure on the spending plans of countless American households.
The most intuitive method sellers in a market can wield power is when the marketplace is reasonably concentrated, with too few sellers to supply significant price competition. This absence of competitors is an obvious function of those corners of the healthcare market that are explicitly safeguarded by patents (pharmaceuticals and medical instruments, mainly), as explained above - what role do lobbyists play in health care policy decisions.
This debt consolidation has been both horizontal and vertical. Horizontally, the variety of hospitals (or healthcare facility business) in Mental Health Facility any given region is falling on average gradually, and this fall has actually restricted rate competitors. Vertically, healthcare facilities have actually associated with other companies (typically networks of doctors) to extend pricing power. The year 2017 saw a record number of medical facility mergers and acquisitions (115 ), and 2018 saw 30 such mergers and acquisitions in the very first quarter alone.
In 2007, 53 percent of community healthcare facilities came from a bigger system. By 2017, the share was over two-thirds (66.8 percent). Likewise, in between 2009 and 2015, the share of hospital-employed physicians grew from 40 to 48 percent - how does universal health care work. Research shows that medical facility mergers increase the price charged for services by 1017 percent.
Other research study indicates that when medical facilities get physician practices, rates for physican services increase by 14 percent. A growing literature has actually recorded possible increases in market concentration across a series of sectors and geographies. This broader literature makes an effective case that boosted antitrust protection must be a crucial concern of economic policymakers in coming years.
No one who was clear-eyed about the deep issues in the American health system in 2009 thought that the Affordable Care Act ought to be the last ambitious reform undertaken. While the ACA was a major step forward in addressing some key problemslike the lack of insurance protection among a large share of the populationit was clearly inadequate to work as an extensive treatment for what ailed the American health system.
American healthcare is singularly pricey among industrialized countries, and other countries with a more powerful public role in health provision invest far less while attaining follow this link at least similar (and typically exceptional) health results. This insight is what lies behind the substantial political desire to have the United States embrace a "single-payer" healthcare financing program.
Health Care Policy - An Overview - Sciencedirect Topics - Truths

Luckily, however, much of the crucial policy provisions that enable more robust public systems to achieve higher expense containment without compromising quality can be adopted quite early in any march toward single-payer. These cost-containment strategies would not only make a large public role for healthcare more plausible, they would likewise provide much-needed relief in the short go to the personal American healthcare system, especially the system of employer-provided health care.
These homes with ESI plans have actually shown themselves to be (not surprisingly) rather hesitant about major reforms that threaten to interrupt this system before a tested alternative is demonstrated. As this report reveals, nevertheless, there are considerable reforms we can enact that would both lead the way for single-payer reform in the long run and, in the short run, provide enormous advantages for those families who currently have ESI Drug and Alcohol Treatment Center coverage.
I also thank Krista Faries and Lora Engdahl for modifying support. Large portions of the section detailing the dangers of policy procedures to assault usage are lifted from Gould 2013, which in turn draws greatly on previous joint work. signed up with the Economic Policy Institute in 2002 and is currently EPI's director of research study.
He has actually authored or co-authored three books (consisting of The State of Working America, 12th Edition) while operating at EPI, edited another, and has composed many research study documents, consisting of for academic journals (what is trump's policy on health care). He appears frequently in media outlets to provide economic commentary and has affirmed numerous times prior to the U.S. Congress.
The Only Guide to Health Policy - Wikipedia
Table of ContentsAn Unbiased View of The Role Of Public Policy In Health Care Market Change ...Some Ideas on United States - Commonwealth Fund You Need To KnowThe 20-Second Trick For United States - Commonwealth Fund
However, even if Medicare compensation rates Drug and Alcohol Treatment Center supply useful information to personal insurance providers, this latter group's success in achieving the same bargain Medicare strikes with suppliers will depend on raw market power. As a current landmark research study of the personal insurance coverage market (Cooper et al. 2018) put it, "The results paint a constant image of bargaining power.
One apparent method to assist the pricing standards set by Medicare use more securely to all private payers (even those not large enough to wield considerable bargaining power by themselves) is to develop all-payer rates. All-payer rates, just like they sound, merely require that health care service providers charge the same price for a given procedure regardless of who is spending for it.
2018). It is tough to see how this variance assists effectiveness, and mindful research has concluded that it is largely the result of differential bargaining power wielded by various health care payers. Setting all-payer rates efficiently lets the payer with one of the most bargaining power set rates for everybody. It therefore duplicates much of the monopsony power of big public systems.
Murray (2009) has recorded that hospital prices in Maryland have risen even more slowly than in other states in recent decades, indicating some useful impact of all-payer rates. A growing share of health expenses in recent years is represented by increased spending on pharmaceuticals. These drugs are generally developed and tested by personal companies that are offered copyright rights, which in turn provide them significant monopoly prices power.
This recommends highly that other countriesagain, frequently with the assistance of more robust public functions in health financinguse their buying power to lower the pharmaceutical business markups on drugs. Strikingly, Medicare was clearly disallowed from successfully working out for lower drug prices when the 2003 law that expanded Medicare coverage to consist of pharmaceuticals was passed.34 Affirming Medicare's responsibility to strike much better bargains for taxpayers when buying from pharmaceutical business need to be seen as low-hanging fruit in the battle to control expenses.
Baker (2008) would go even further than just having the government anticipate lower costs when serving as a direct buyer. He recommends having clinical trials for brand-new drugs be publicly financed. what is the affordable health care act. He keeps in mind the numerous financial disputes of interest that emerge when drug business themselves carry out and report on the outcomes of clinical drug trials.
Baker advises that the expense of establishing openly financed drug trials be recovered (and then some) by having the intellectual residential or commercial property arising from brand-new discoveries be put in the public domain. This would result in far lower prices charged for pharmaceuticals. Finally, the massive price differences throughout nations (even those that share a border) for the exact very same brand name of drug recommends one obvious potential strategy for decreasing drug expenses in the United States: Allow these drugs to be purchased in other countries and reimported into the United States.
Not known Facts About U.s. Health Care Policy - Rand
Yet these very same trade treaties have generally forbidden such drug reimportation and even demanded extension of U.S. levels of copyright protections to trading partners as a prerequisite for access to the U.S. market. This is a truly odd oversight on the part of the professionfree trade in pharmaceuticals would really solve a pressing economic pressure on the budget plans of millions of American households.
The most user-friendly method sellers in a market can wield power is when the market is reasonably focused, with too couple of sellers to provide meaningful price competitors. This absence of competitors is an obvious function of those corners of the healthcare market that are clearly protected by patents (pharmaceuticals and medical instruments, mainly), as explained above - what is health care policy.
This consolidation has been both horizontal and vertical. Horizontally, the variety of medical facilities (or healthcare facility companies) in any given region is falling on average in time, and this fall has restricted cost competition. Vertically, health centers have actually affiliated with other service providers (often networks of physicians) to extend pricing power. The year 2017 saw a record variety of health center mergers and acquisitions (115 ), and 2018 saw 30 such mergers and acquisitions in the very first quarter alone.
In 2007, 53 percent of community health centers belonged to a bigger system. By 2017, the share was over two-thirds (66.8 percent). Likewise, in between 2009 and 2015, the share of hospital-employed physicians grew from 40 to 48 percent - what is required in the florida employee health care access act?. Research study shows that healthcare facility mergers increase the cost charged for services by 1017 percent.
Other research indicates that when healthcare facilities acquire doctor practices, rates for physican services increase by 14 percent. A growing literature has actually recorded prospective boosts in market concentration across a series of sectors and locations. This larger literature makes an effective case that enhanced antitrust defense ought to be an essential priority of financial policymakers in coming years.
Nobody who was clear-eyed about the deep problems in the American health system in 2009 thought that the Affordable Care Act ought to be the last ambitious reform carried out. While the ACA was a major action forward in attending to some key problemslike the lack of insurance protection amongst a big share of the populationit was plainly insufficient to function as a detailed cure for what ailed the American health system.
American health care is singularly costly follow this link amongst industrialized nations, and other countries with a stronger public role in health provision invest far less while attaining at least comparable (and often remarkable) health results. This insight is what lies behind the considerable political desire to have the United States embrace a "single-payer" health care funding program.
Healthcare Policies - List Of High Impact Articles - Ppts ... for Beginners
Thankfully, nevertheless, much of the key policy arrangements that allow more robust public systems to attain higher expense containment without sacrificing quality can be adopted rather early in any march toward single-payer. These cost-containment methods would not only make a big public role for health care more possible, they would also supply much-needed relief in the short run to the personal American healthcare system, especially the system of employer-provided healthcare.

These families with ESI plans have shown themselves to be (understandably) quite hesitant about major reforms that threaten to disrupt this system prior to a tested alternative is demonstrated. As this report shows, however, there are significant reforms we can enact that would both pave the method for single-payer reform in the long run and, in the short run, provide massive advantages for those households who currently have ESI coverage.
I also thank Krista Faries and Lora Engdahl for modifying support. Large parts of the section detailing the risks of policy procedures to assault utilization are raised from Gould 2013, which in turn draws greatly on previous joint work. Mental Health Facility joined the Economic Policy Institute in 2002 and is currently EPI's director of research study.
He has authored or co-authored three books (including The State of Working America, 12th Edition) while operating at EPI, edited another, and has composed many research study papers, including for academic journals (if you were to promote a dental health policy). He appears typically in media outlets to use economic commentary and has actually affirmed several times before the U.S. Congress.
